FAQ
Helpful Information About Dr. Brem’s Medical Care Treatments
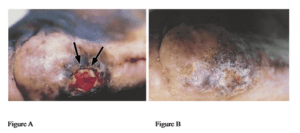
Figure A: Diabetic foot ulcer in the lateral metatarsal area present for 14 months. Patient had the other leg amputated secondary to wound complication. Photograph taken in office 1 week after human skin equivalent was placed. Arrows point to where sutures were placed and demonstrate a considerable amount of contraction in only 1 week.
Figure B: One month after an application of human skin equivalent, the diabetic foot ulcer was healed completely.
The American Journal of Surgery 188 (Suppl to July 2004) 9S–17S
Protocol for the successful treatment of pressure ulcers.
Harold Brem, M.D.
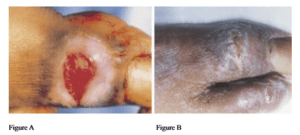
Figure A: Diabetic foot ulcer in the unusual location of the dorsal surface of the first toe. After a single application of Apligraf (synthesized by Organogenesis Inc, Canton, Mass, and distributed by Novartis Pharmaceuticals Corp, East Hanover, NJ) applied in the standard fashion, the wound was healed completely and epithelialized.
Figure B: Picture taken 8 weeks after a single application.
The American Journal of Surgery 188 (Suppl to July 2004) 9S–17S
Protocol for the successful treatment of pressure ulcers
Harold Brem, M.D.
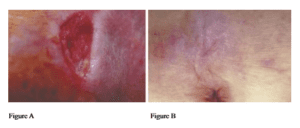
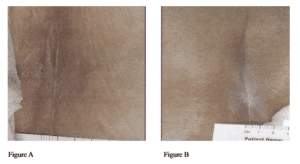
Figure A: Quadriplegic who had a non-healing sacral ulcer. In this photograph, the wound was debrided down to subcutaneous tissue.
Figure B: His wound healed 3 weeks after application of the skin graft, 1 week before the photograph was taken.
The American Journal of Surgery 188 (Suppl to July 2004) 9S–17S
Protocol for the successful treatment of pressure ulcers
Harold Brem, M.D.
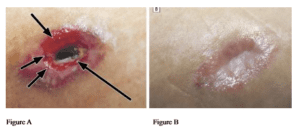
Figure A: Three days after Apligraf was sutured into a pressure ulcer with depth in the right trochanteric area of 2.8 cm. Short arrows point to sutures. Long arrow points to human skin equivalent.
Figure B: Seven weeks later, it filled in with granulation tissue and had fully epithelialized, suggesting the effectiveness of Apligraf in forming granulation tissue and aiding in epithelialization.
The American Journal of Surgery 188 (Suppl to July 2004) 9S–17S
Protocol for the successful treatment of pressure ulcers
Harold Brem, M.D.
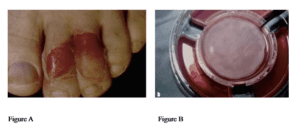
Healing of a diabetic toe ulcer.
Figure A: Diabetic patient with toe ulcers before treatment with bilayered living human skin equivalent (HSE).
Figure B: HSE, as it arrives in Transwell, immediately before application.
What is the healing time for HSE in diabetic toe ulcers?
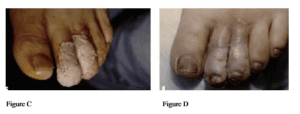
Figure C: Same toe ulcers, immediately following application of HSE.
Figure D: Toe ulcers healed in 35 days.
Clinical Efficacy and Mechanism of Bilayered Living Human Skin Equivalent (HSE) in Treatment of Diabetic Foot Ulcers
Harold Brem, M.D., Jan Young, Ph.D., Cary Isaacs, M.S., Marjana Tomic-Canic, Ph.D
H. Paul Ehrlich, Ph.D.
Pressure ulcers present with many etiologies. In the protocol outlined, the treatment is almost always the same regardless of etiology. Specifically, it is the basis of this protocol that all-new pressure ulcers be treated immediately upon recognition.
Figure A: A 91-year-old woman with a sacral ulcer. This patient was treated immediately, and subsequently, her venous stasis ulcer healed rapidly (Figure B) under the protocol. No debridement or culture was needed. This is a typical example of how early treatment halts ulcer progression. This patient became progressively wheelchair-bound and was instructed to report any new break in the skin. Almost all pressure ulcers present in a similar fashion, i.e., as a break in the skin.
What should the protocol be for bed-bound or wheelchair-bound patients to prevent any type of wound?
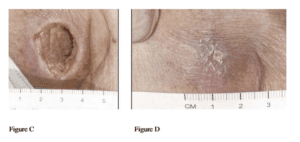
Figure C: In contrast to the case depicted above in Figures A and B, this previously healthy 96-year-old man had also become progressively wheelchair-bound but presented with an infected stage IV pressure ulcer requiring operative debridement. He healed on the protocol (Figure D) but would have avoided the morbidity and expense of a stage IV ulcer if he had presented upon first recognition. This case also emphasizes that every wheelchair- or bed-bound patient must be examined daily and the protocol initiated immediately upon recognition of a break in the skin.
The American Journal of Surgery 188 (Suppl to July 2004) 9S–17S
Protocol for the successful treatment of pressure ulcers
Harold Brem, M.D., Jan Young, Ph.D., Cary Isaacs, M.S., Marjana Tomic-Canic, Ph.D.
H. Paul Ehrlich, Ph.D.
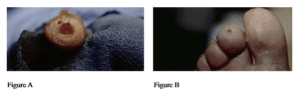
Figure A: Toe ulcer of a 70-year-old man with type-2 diabetes, first seen with an infected cellulitis toe ulcer. This figure depicts the wound after intravenous antibiotics and surgical debridement.
Figure B: Patient’s toe ulcer healed after early comprehensive treatment. There should never be an exception to proper wound-bed preparation (i.e., early surgical debridement in a diabetic foot ulcer and treatment with antibiotics targeted directly toward bacteria growing from the deep culture) because a patient is elderly. The elderly can heal if provided with early intervention and comprehensive care.
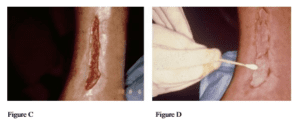
Figure C: 82-year-old patient with diabetes first seen with a venous stasis ulcer of an 18-month duration that started after a vein was harvested for coronary arterial bypass grafting. Costs for daily nursing visits regarding this patient’s wound treatment alone totaled over $70,000. Doppler ultrasound confirmed venous reflux. No data exist that patients with diabetes and venous reflux have a different rate of healing.
Figure D: Note bilayered human skin equivalent (HSE) (cultured keratinocytes and fibroblasts on type-1 collagen) being applied to the venous ulcer. Application was administered in an office setting with a 1-mm distance left between debrided healing skin edge and new bilayered HSE.
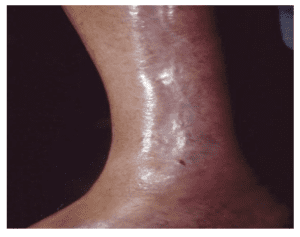
Figure E: Venous stasis ulcer healed at 7 weeks.

Figure F: Wound is contracting and epithelializing. Important to note is that even ischemic, infected wounds in the elderly (this patient also had venous reflux and took systemic steroids) are expected to heal as long as comprehensive treatment is initiated immediately.
Harold Brem, M.D., Alina Tarnovskaya, B.A., Edwin Baskin-Bey, M.D., Miriam Carsa, ED.D., C.N.A., Hyacinth Entero, B.A., Marjana Tomic-Canic, Ph.D., H. Paul Ehrlich, Ph.D., Kiran Gill, B.A., Sarah Weinberger, D.E.C.
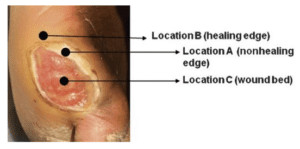
As debridement progresses and the non-healing edge is removed, the part of the wound edge is reached, that contains cells capable of migration and participation in wound healing. The clinician’s challenge is how to identify this region and determine the proper debridement margin.
Adv Skin Wound Care. 2008 October; 21(10): 487–494. doi:10.1097/01.ASW.0000323563.59885.1c.
Using Gene Transcription Patterns (Bar Coding Scans) to Guide Wound Debridement and Healing Marjana Tomic-Canic, PhD, Elizabeth A. Ayello, PhD, Olivera Stojadinovic, MD, Michael S. Golinko, MD, Harold Brem, MD