Providing Medical Care Services With Compassion
Treating Chronic Wounds
All of Dr. Brem's wound patients are treated with multiple therapies that include state-of-the-art wound treatments‑based on analysis of his or her wound tissue‑as well as comprehensive care of the patient’s underlying medical issues. Through the integrated, simultaneous use of various regenerative medicine techniques, even chronic wounds can be encouraged to heal. The key elements of this
Patient Evaluation
Dr. Brem's integrated wound healing approach to wound care begins with the patient’s first visit, which may include examinations by a range of physician specialists. Depending on the patient’s condition, these may include a general surgeon, a plastic surgeon, an orthopedic surgeon, and/or a vascular surgeon, as well as specialists in nephrology, podiatry, cardiology, infectious diseases, diabetes, neurology, gastrointestinal disorders, pain management, and geriatric medicine. These specialists will then combine their findings to develop a comprehensive treatment plan.
The Initial Patient Evaluation
Also includes tests for blood chemistry (including blood lipids and blood glucose levels), blood flow in the limbs, kidney and thyroid function, and nutritional status. Since each of these factors can influence a wound’s ability to heal, the results of this comprehensive evaluation will help guide the patient's treatment plan.

Treating Related Medical Conditions
Chronic wounds usually involve other related medical conditions that work to impair the healing process. As part of his integrated approach to wound healing, Dr. Brem works closely with other specialists to identify and address any such medical conditions, including the following:
Diabetes. Working with a diabetes specialist to manage the patient's blood glucose levels helps accelerate the healing process and prevent new diabetic wounds from developing.
Neuropathy. Diabetes-related nerve damage in the legs and feet is a key contributor to diabetic foot ulcers. A surgical technique called nerve decompression can help this condition.
Impaired peripheral blood flow. Reduced blood circulation in the legs due to arterial plaque is a major reason why leg and foot wounds fail to heal. In these cases, bypass surgery or angioplasty to restore blood flow to the affected area can often help the healing process.
Venous insufficiency. This condition, in which blood becomes “backed up” in the veins, is associated with varicose veins and can also cause venous ulcers to form. Once a venous ulcer has begun healing, working to resolve the underlying problems with blood flow through the veins can help prevent a recurrence.
Cardiovascular disease. Conditions such as atherosclerosis, hypertension, or arrhythmia can often impair blood flow to a patient's wound, impairing the healing process. In these cases, Dr. Brem and his team work closely with the patient’s cardiologist to treat the underlying condition.
Kidney disease. Impaired kidney function, a common complication of diabetes, can also impede wound healing. If tests of a patient’s kidney function reveal abnormalities, Dr. Brem will work closely with a nephrologist (kidney specialist) to address the condition.
Skin trauma. For patients with diabetic foot ulcers or pressure ulcers (also known as bed sores), taking pressure off the affected skin area is an essential step in enabling the wound to heal and preventing new wounds from forming.
Nutritional issues. Proper nutrition is key to the wound healing process. Dr. Brem and his team evaluate each patient’s nutritional status and provide nutritional supplementation to address any deficiencies that are identified.
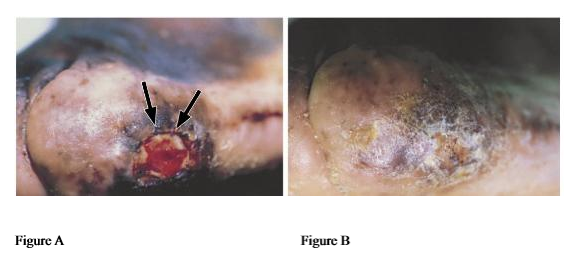
Debridement of Wound Tissue
Debridement, in which a wound physician removes dead, infected, or non-healing tissue, as well as scar tissue and calluses, is a key part of the wound healing process. There are various debridement techniques, but the most effective method, and the one typically used by Dr. Brem, involves surgical debridement
Debridement accelerates the healing process by eliminating tissue that is hindering the healing process, and by stimulating the release of growth factors at the wound's edge of the wound. Once the non-healing tissue is removed, antibiotics are administered to the wound site as needed along with regenerative medications to stimulate the growth of healthy
During each procedure, Dr. Brem's team also conducts a cellular analysis of the tissue being debrided to determine exactly how much tissue to remove. This enables us to maximize the benefits of each procedure, reducing the total number of
With some patients, a single debridement procedure is enough to promote complete healing of the wound. With other patients, multiple debridements may be needed. Debridement is generally done on an outpatient basis and takes an hour or less. In some cases, regional anesthesia can be used during debridement in place of general anesthesia—an approach Dr. Brem has helped pioneer.
Biological Analysis of the Wound
As part of Dr. Brem's integrated approach to wound healing, he will order a lab analysis of a patient's wound tissue samples obtained during the debridement process. This analysis includes checking for abnormalities in the tissue's molecular makeup or structure, to help pinpoint which regenerative therapies will be most effective, and testing for various bacteria and fungi, to determine the scope of any infection that may be present and identify which antibiotics to administer.


Treating Infection
Chronic wounds are highly prone to infection, which interferes with the wound healing process. For this reason, eliminating any underlying infection is an essential part of Dr. Brem's wound treatment protocol. Surgical debridement of the wound to physically remove infected wound tissue is an important element of this process.
If analysis of the debrided wound tissue indicates that bacterial infection is still present, the patient will be treated with antibiotics tailored to that particular bacteria strain, including intravenous antibiotics and/or oral antibiotics as needed. If the infection persists despite antibiotic therapy, Dr. Brem may do additional debridement procedures until the infection has been eliminated.
Employing Regenerative Medicine
The use of regenerative medicine is an essential part of Dr. Brem's integrated wound healing approach. Dr. Brem has helped pioneer many of these treatments and has unsurpassed expertise in using them to spur the formation of healthy cells and neutralize the factors that prevent chronic wounds from healing.
Following surgical debridement of the wound, regenerative medicine is administered directly into the wound tissue. Since every patient's wound has a unique biological profile, Dr. Brem also analyzes tissue cultures taken from each patient’s wound to determine which combination of regenerative medications will be most effective.


Following are some of the regenerative therapies commonly used by Dr. Brem and his wound healing team:
• Apligraf (Human Skin Equivalent)
• Leukine (Granulocyte-Macrophage Colony-Stimulating Factor, or GM-CSF)
• Other Growth Factors: PDGF-BB and VEGF
• Platelet-Rich Plasma (PRP)
• Stromal Vascular Fraction Cells (Stem Cells)
• Extra-Cellular Matrix
• Negative Pressure Therapy
Hyperbaric Oxygen Treatments
Another important tool in Dr. Brem's treatment of chronic and complex wounds is hyperbaric oxygen therapy. In selected patients, this approach can provide the extra boost that enables problem wounds to start healing, especially when combined with regenerative medicine therapies.
In order for any wound to heal, it needs to receive an adequate blood flow, bringing in healing oxygen and nutrients as well as antibodies that fight infections, and removing toxins that impair healing. An impaired blood supply is often a contributing factor when a chronic wound fails to heal properly.
In hyperbaric oxygen therapy, the patient relaxes inside the hyperbaric chamber, breathing in pure oxygen under an air pressure significantly higher than that of sea level. This elevated pressure causes significantly more oxygen to be taken up by the bloodstream and carried to the wound tissue, spurring the growth of new blood vessels in the affected tissue and giving a boost to the healing process.
Wound patients receiving hyperbaric oxygen therapy typically undergo 20 to 40 treatment sessions, lasting about two hours each.
Monitoring the Healing Process
Since chronic wounds typically take months to heal, even with highly effective treatment, Dr. Brem and his team closely monitor each patient's healing process—an approach that Dr. Brem has helped to pioneer. This includes maintaining a photographic record of the wound, which is combined with other key information about the patient’s health status into a single-screen online document.
This information is reviewed by Dr. Brem on a regular basis and is also made available to other members of the patient's medical team. Each patient's online wound electronic medical record also generates automatic alerts if a patient’s condition shows signs of worsening—ensuring that needed interventions are carried out in a timely and effective fashion.
